It's a subject many dance around, but let's get real about aging, masculinity, and the elephant in the room: declining testosterone levels. If you're over 30 and a man, here's the unsweetened scoop.
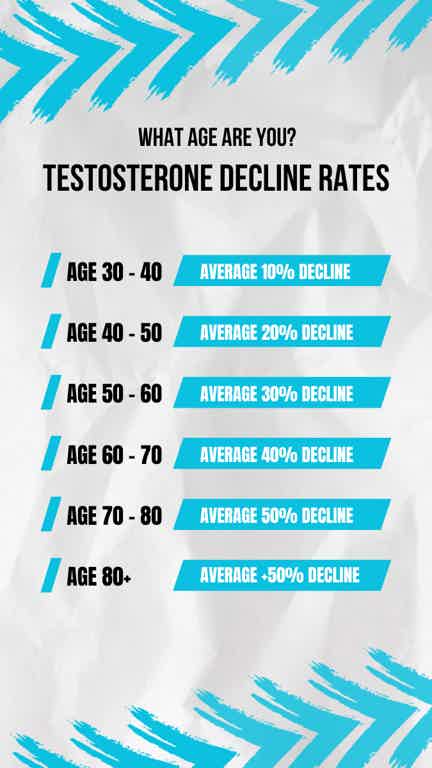
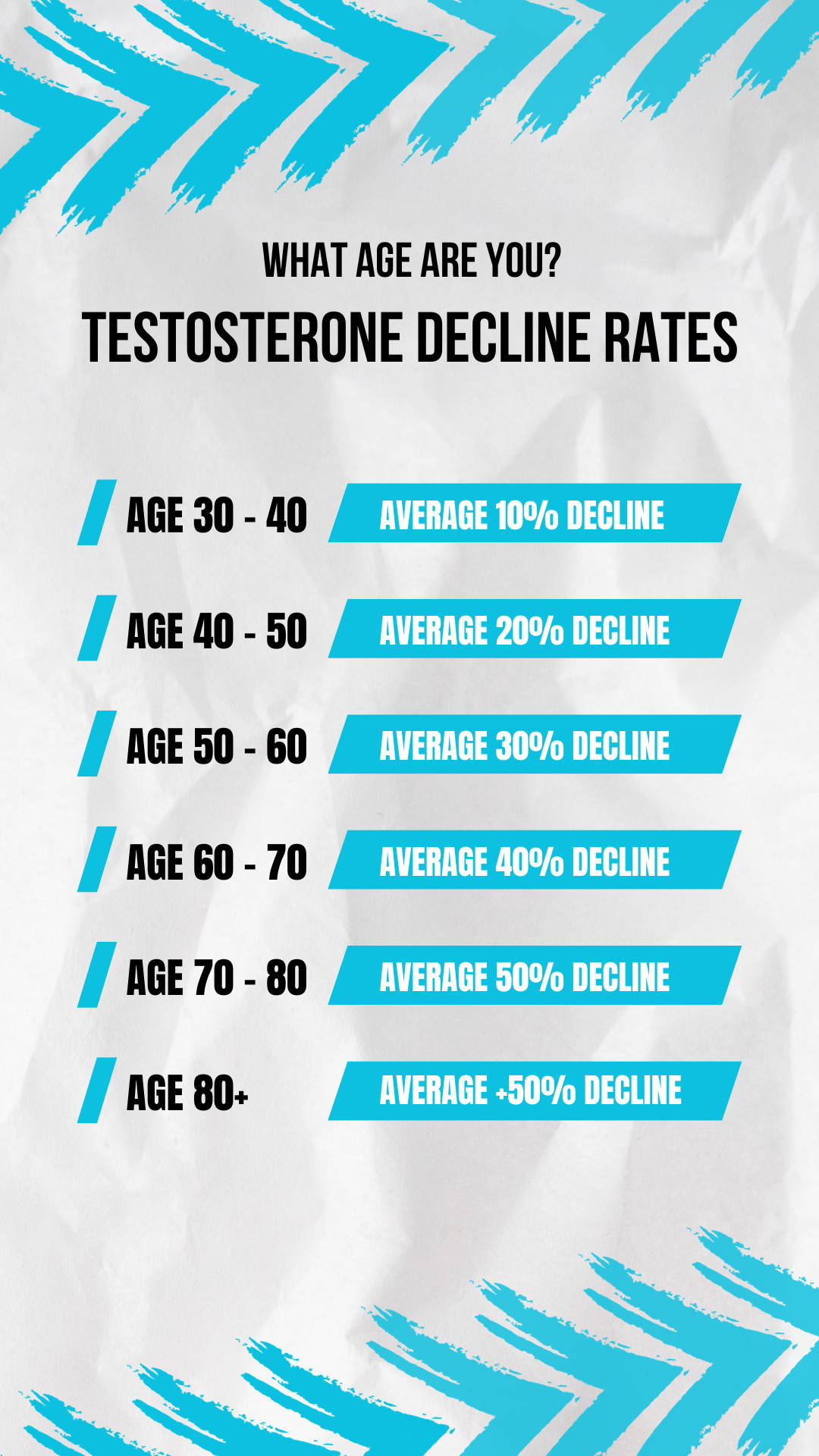
Nature's Downward Slope: Starting from your late 20s to early 30s, your testosterone levels dip roughly 1% each year. It's a natural part of aging, but it has profound effects on your energy, libido, muscle mass, and even your mental focus.
Not Just a Bedroom Problem: Sure, lower testosterone can impact your sex drive and performance, but it's not only about that. The effects are more comprehensive—think reduced muscle tone, increased body fat, bouts of fatigue, and even mood swings or depressive episodes.
Your Workout Isn’t Enough: While exercise can help boost testosterone to some extent, relying solely on your gym routine as you age can be an exercise in futility. As your natural testosterone levels decrease, the same efforts in your 30s and 40s might not yield the results they once did in your 20s.
The Modern Lifestyle Assault: Stress, poor diet, lack of sleep, and certain medications can further deplete your testosterone. The modern man is up against a wall of factors that weren't as prevalent for previous generations.
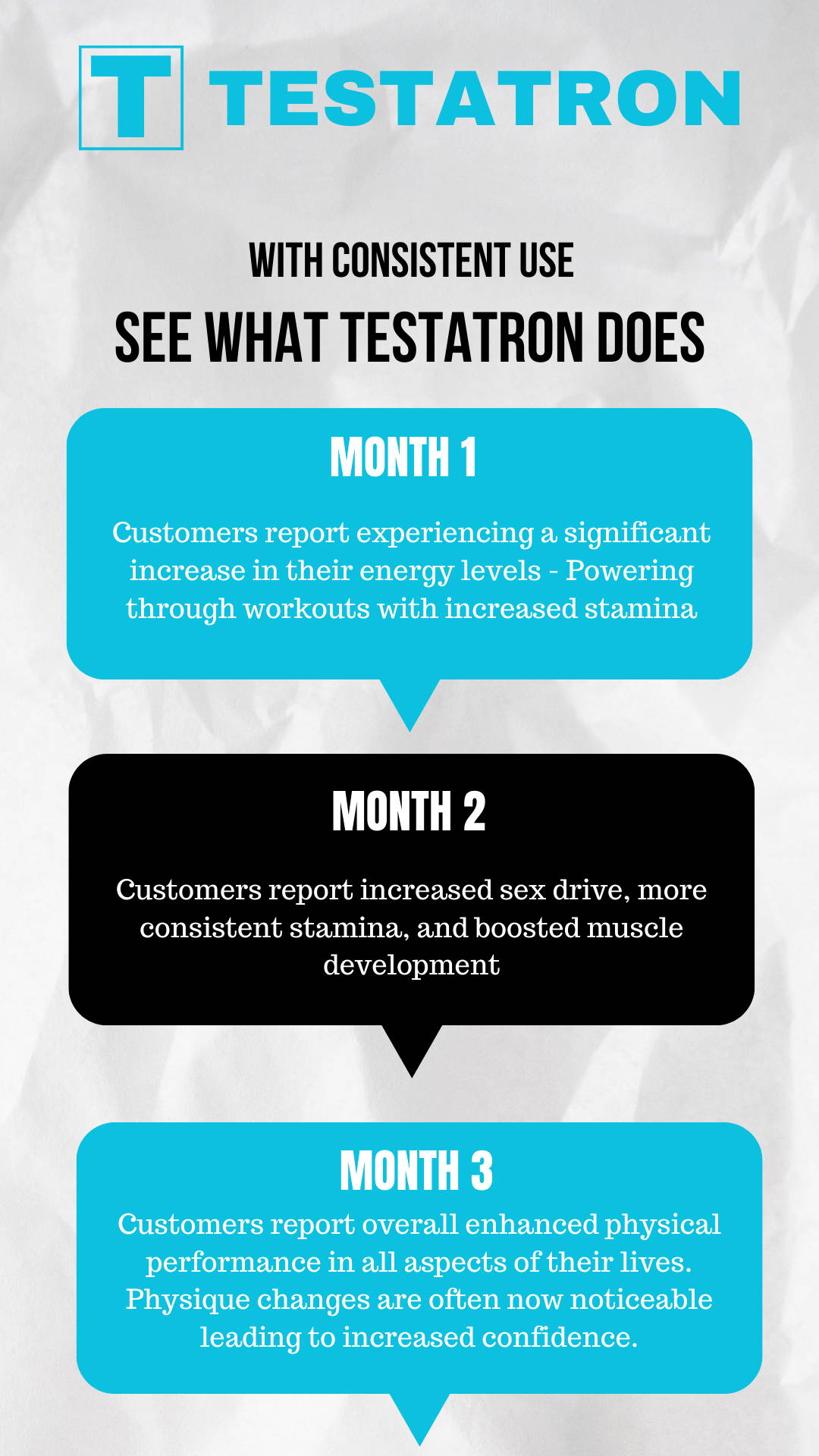
Not All Boosters Are Steroids: There's a stigma around testosterone boosters that they're akin to steroids. The truth? Many boosters, like natural supplements, work by supporting your body's own ability to produce testosterone, not by introducing synthetic hormones.
It's a Quality of Life Issue: This isn't just about looking good shirtless or impressing someone in the bedroom. Balanced testosterone levels can mean better mental clarity, improved mood, healthier bone density, and an overall enhanced quality of life.
In the end, the brutal truth is this: aging is inevitable, but how we age is, to a significant extent, a matter of choice. Embracing tools like testosterone boosters isn't about chasing lost youth; it's about maximizing health, vitality, and well-being at every stage of life.